Frozen Shoulder: Risk Factors And Treatment
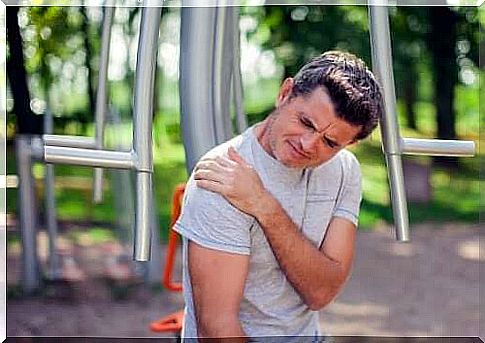
Frozen shoulder is a pathological and trauma condition affecting the shoulder joint. It is also known as adhesive capsulitis, as the ultimate manifestation of symptoms is inflammation of the shoulder capsule.
To understand this mechanism, we would have to review this skeletal structure. It is a joint that acts as a point of union of three important bones: the humerus, the clavicle and the scapula, surrounded by a soft tissue that creates a capsule and wraps them. This capsule is the part that becomes inflamed in the case of the frozen shoulder.
It is estimated that around 2% of the world’s population suffers from it at some point in their life. It occurs mainly between the ages of forty and sixty, with a greater impact on women.
As we will see later, there are people who are more at risk than others, and this is mainly associated with a lack of movement, which leads to stiffening of the joint capsule. It is no coincidence, in fact, that it is often diagnosed in hospitalized patients.
Frozen Shoulder Symptoms and Diagnosis
The frozen shoulder has a slow course: the symptoms, that is, do not appear overnight. It is characterized by three phases, which can take up to four years to manifest itself. Below, we describe the process:
- Motor block: it is the first phase of the pathology and is characterized by the pain accused when moving the shoulder. Although it is still possible to move the joint, the person notes that the mobility is limited. This period can last from two to nine months.
- Freezing: This second phase is also known as the stiffness phase. It becomes very difficult to move the shoulder, even to carry out normal daily activities. This phase lasts from one to six months.
- Thawing: it is a phase of symptom improvement, whether by natural course or by intervention with medical therapies. Complete recovery can take anywhere from six months to two years.
To make the diagnosis, the doctor must perform a thorough clinical examination, as the symptoms are clear. Usually, the practitioner takes the sore upper limb and tries to move it in different directions.
When the doctor moves the patient’s shoulder without asking the patient to exert force, he measures the degree of passive movement. In addition, he will ask the patient to move his arm as much as possible in order to assess the level of active movement. In the case of the frozen shoulder, both ranges of motion – passive and active – are limited and painful.

Risk factors
Frozen shoulder is associated with situations where mobility is reduced. For example, if you stand still for a long time, you run a greater risk. It may happen that there is no complete decubitus, but little mobility of the upper limb due to some trauma, and the effect will be the same.
Some of the risk factors for poor mobility are:
- Age: very old people who need outside help to get around.
- Fractures in the arm or forearm, resulting in the placement of the cast.
- Cerebrovascular accident (stroke): The entire recovery period from strokes is slow and characterized by poor mobility.
- Post-operative: invasive surgical interventions that force the patient to rest for a long time.
Among the risk factors we must also include a group of diseases which, without requiring decubitus, have been identified as possible causes of predisposition to frozen shoulder. Among them:
- Diabetes: Scientific studies have found that up to 20% of patients with diabetes suffer from frozen shoulder at some point, although the cause is not known.
- Anomalies of the thyroid gland: hypothyroidism and hyperthyroidism.
- Parkinson’s disease.
Treatment of the frozen shoulder
Most patients with frozen shoulder can improve with anti-inflammatory treatments and physiotherapy. Typically, 90% of patients do not need to undergo corrective surgery.
Among the prescription drugs, we find non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids. The most frequently chosen NSAID is ibuprofen. As for corticosteroids, on the other hand, cortisone is preferred, to be injected directly into the painful joint.
Physiotherapy is also essential, in fact there are certain exercises and specific maneuvers that are effective in the case of a frozen shoulder. Generally, they are combined with the application of heat to obtain a loosening of rigid structures.
Ultimately, the surgical option is reserved for those patients who do not respond well to non-invasive options, namely drug treatment and physiotherapy. It doesn’t represent the majority of cases, as mentioned, but this option exists. There are two surgical maneuvers:
- Manipulation : Under anesthesia, medical personnel move the shoulder forcing it, which results in rupture of the hard capsule and release of the joint.
- Arthroscopy: the surgeon cuts out some parts of the stiffened capsule through small incisions made with special tools for the purpose.
To conclude
Frozen shoulder can become disabling and very painful. If you recognize similar symptoms, such as difficulty moving your shoulder or carrying out activities of daily living, the best thing to do is consult a doctor who can make the correct diagnosis.