Vascular Perforation From Central Venous Catheter
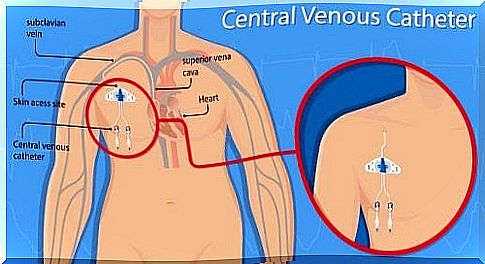
Vascular perforation from a central venous catheter occurs when the tip of the catheter is moved. It can happen at any level and regardless of where the other end is located.
However, such perforation is a rare complication. Only 10% of perforations occur in the central veins; correct diagnosis is usually late, contributing to a high risk of mortality.
Ultrasounds are applied to allow the radiologist to detect the most suitable veins for the placement of the catheter.
Types of vascular access catheters and vascular perforation

Unlike the catheter used in the standard intravenous mode, a vascular access catheter is more durable and does not clog or become infected easily.
This type of catheter is designed to extend into the largest central vein near the heart. Catheters vary in size, width and number of channels, depending on the use for which they are intended. Below, we see the main types of vascular access catheters:
Central catheter with peripheral insertion and risk of vascular perforation
It is a long catheter that extends from a vein in the arm or leg to the inside of the largest vein close to the heart. These catheters are called midline when they are positioned in such a way that the tip flows into a relatively large vein. However, it does not extend into the larger central vein.
Central catheter not tunneled
The non-tunneled central catheter may be of larger caliber and is designed to be placed in a relatively large vein. Furthermore, this vein is more central, as is the jugular vein in the neck or the femoral vein in the groin.
Tunneled catheter
It may have a “sleeve” that stimulates the growth of tissue that helps keep it in place in the body. There are different sizes and types of tunneled catheters. Characteristics of the tunneled catheter are the fact that it is safe and easy to access.
Port catheter
It is a permanent device which consists of a catheter coupled to a small reservoir.
Risk of vascular perforation
Placement of a peripheral insertion central catheter can be associated with serious complications. Among them the vascular perforation, for which the correct positioning must always be verified.
The diagnostic test of choice for central vascular perforation is contrast computed tomography. There are two types of risks associated with vascular access catheters; those that can occur during the insertion procedure and those that occur because the device is inside the body. These risks include:
- Infection at the site of the incision shortly after placement of the catheter.
- Risk of bleeding.
- Pneumothorax: an accumulation of air in the chest, which can cause the collapse of one of the two lungs. This can occur when placing the catheter via a vein in the chest or neck, but does not occur if a vein in the arm is used.
- On rare occasions the catheter enters an artery rather than a vein. Should this occur, the catheter would need to be removed. Most of the time the artery will heal on its own, but sometimes surgical repair is required.
Late infection associated with the vascular access catheter
Following the insertion of a vascular access catheter, two types of late infection can occur: skin infection involving the catheter insertion site or bloodstream infection.
When the catheter is not well inserted into the skin, there is a possibility that it may accidentally come out. If this occurs, pressure should be applied to the incision site with sterile gauze and the physician should be notified as soon as possible.
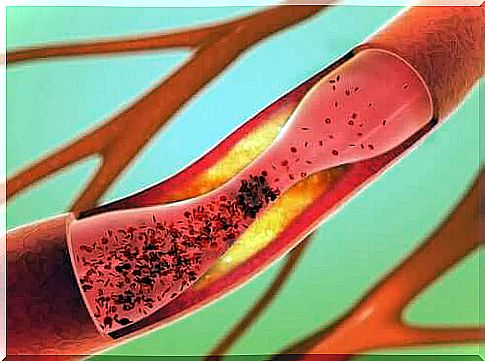
Also, any type of vascular access catheter could become blocked with a blood clot. The clot can be treated with a blood-thinning drug, but in some cases you will have to proceed by pulling out the catheter.
On the other hand, in rare cases, patients experience a sensation of an irregular heartbeat. This sensation can be associated with the catheter.